The American Healthcare System: The Worst System Money Can Buy

The American healthcare system is the worst system money can buy.
In the annals of global economic and technological advancement, the United States stands as a beacon of progress. Yet, beneath this veneer of achievement lies a healthcare system that, despite its considerable resources and capabilities, grapples with a myriad of inefficiencies, access problems, and a shocking decline in life spans.
This article delves deep into the heart of America’s healthcare conundrum, drawing upon data, insights, and analyses from authoritative sources. As we explore the underbelly of a healthcare system that boasts some of the highest expenditure levels worldwide, we uncover the stark realities of a nation that paradoxically struggles to provide quality care and ensure the well-being of its citizens.
A Stagnant State of Public Health:
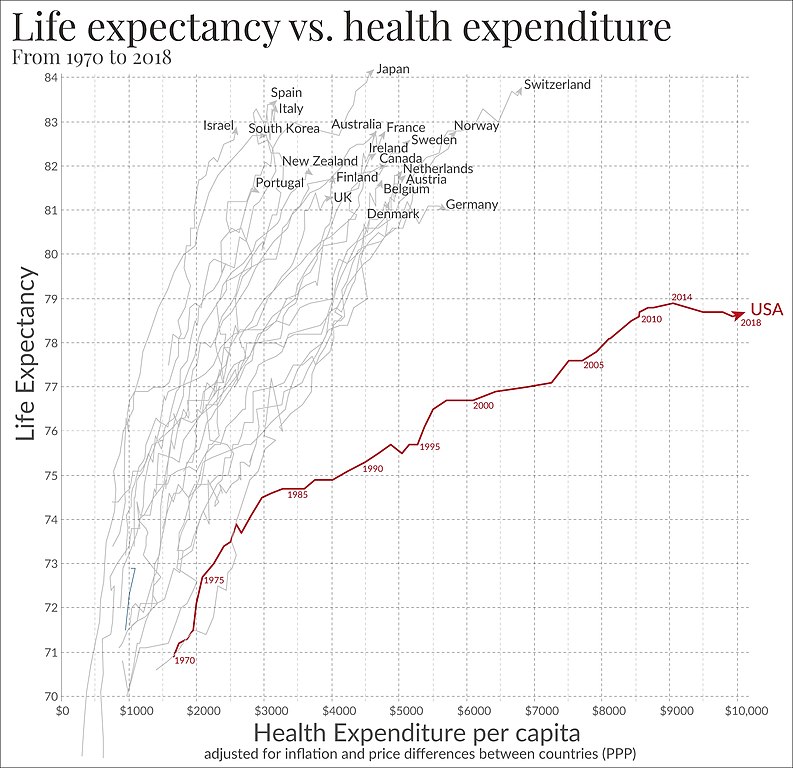
The American healthcare system, despite being one of the most expensive globally, fails to deliver consistent positive outcomes for its citizens. An in-depth analysis by the Commonwealth Fund paints a clear picture of this paradoxical situation. In the realm of healthcare spending, the U.S. stands head and shoulders above other wealthy countries, shelling out a staggering 16.9% of its GDP on health services. To put this in perspective, Switzerland, the second-highest spender, allocates a relatively modest 12.2% of its GDP.
However, this significant investment does not seem to translate to better health for Americans. Among 11 high-income countries studied, the U.S. sits at the bottom of the pile in life expectancy, with citizens expected to live 78.6 years on average. This is stark when juxtaposed against nations like Switzerland and Japan, where life expectancy stretches beyond 83 years.
Adding salt to the wound is the looming burden of chronic diseases. In the analysis, a significant 68% of adults aged 65 and over in the U.S. reported having two or more chronic conditions, underscoring the scale of health challenges. This figure was considerably higher than in other countries; for instance, only 33% of older adults in the UK reported two or more of such conditions.
The healthcare system’s inefficiencies become even more evident when considering avoidable hospital admissions. Asthma and diabetes, conditions that can typically be managed outside a hospital setting with effective primary care, accounted for a sizeable number of U.S. hospital admissions. These admissions, termed “ambulatory care-sensitive condition admission rates,” were notably higher in the U.S. at 156 per 100,000 population compared to countries like Sweden, which had a mere 28 such admissions per 100,000 population.
Taken together, these metrics from the Commonwealth Fund highlight a system struggling to provide value for its considerable expenditures. While the financial investments are evident, the dividends in terms of positive health outcomes for the American population remain troublingly scarce. The data suggests a pressing need to re-evaluate, rethink, and ultimately reform the existing structures and practices of the U.S. healthcare system.
Unraveling the Affordability Crisis:
The complex landscape of healthcare affordability in the U.S. stands out as a pressing concern, exacerbated by seemingly paradoxical factors. Despite hefty investments in the healthcare sector, many Americans find themselves entangled in a web of financial strains related to medical costs.
A study by the Commonwealth Fund unveils that the problem isn’t limited to just the uninsured. Even among the insured working-age Americans, the onslaught of medical bills poses a significant challenge. This is underscored by the fact that 37% of adults decided against a medically prescribed test or treatment in the previous year due to cost concerns. Such decisions, influenced by fiscal constraints rather than well-being, paints a grim picture of the prevailing situation.
The scenario is further complicated by the rising tide of chronic illnesses. With six out of ten U.S. adults battling at least one chronic disease, the continuous expenses related to their condition becomes an inescapable burden. Beyond the immediate costs of treatment, these patients are often saddled with the recurring financial weight of medications, periodic consultations, and other long-term care necessities.
Meanwhile, the United States Congress Joint Economic Committee provides a more granular look at the ramifications of this crisis. An unsettling surge in “deaths of despair,” which encompasses fatalities from alcohol, drugs, and suicides, can be seen in relation to the affordability challenge. The report reveals a notable rise in drug-related deaths, reaching an age-adjusted rate of 20.5 per 100,000 by 2017. These disturbing statistics can be partially traced back to the emotional and financial strain caused by inaccessibility to needed healthcare and treatments.
In a similar vein, the Centers for Disease Control and Prevention (CDC) highlight the long-term consequences of healthcare affordability issues. The tendency to postpone or avoid medical care due to prohibitive costs doesn’t merely lead to immediate health concerns but can precipitate a cascade of complications. This not only amplifies the demand on the healthcare infrastructure but also creates a society hampered by a plethora of untreated or mismanaged health conditions.
In essence, the U.S.’s healthcare affordability crisis transcends mere economic metrics. It’s a multifaceted issue that intertwines with the quality of life, societal well-being, and the overarching ethos of a system that seems to prioritize monetary considerations over genuine health outcomes.
Confronting the “Deaths of Despair”
Amidst the challenges facing the American healthcare landscape, one term stands out in its stark poignancy: “deaths of despair.” This terminology, introduced by the U.S. Congress Joint Economic Committee, encapsulates a deeply troubling facet of American life: a surge in fatalities attributed to alcohol, drugs, and suicide.
These aren’t just isolated incidents or mere statistical outliers; they represent an undercurrent of societal distress that demands attention. The data unveils a troubling chronology. While alcohol-related deaths saw their most disturbing spike in 1974, it’s the narrative of drug-related deaths that evokes profound concern. From the late 1950s onward, the U.S. has seen a consistent and distressing uptick in such fatalities. By 2017, the age-adjusted rate for drug-induced deaths had surged to an unsettling 20.5 per 100,000, as indicated by the U.S. Congress Joint Economic Committee.
The Centers for Disease Control and Prevention (CDC) lends further context to this crisis. Their records point towards a steady rise in suicide rates between 2000 and 2016, with an annual increase of about 1% each year. This lends credence to the overarching narrative of “deaths of despair.” It’s not merely about individuals succumbing to substance abuses or taking their lives; it’s an emblem of the larger psychological and socio-economic challenges grappling the nation.
What drives this surge in despair? Studies suggest a correlation with the burdens of chronic diseases and the economic stresses associated with healthcare. As many grapple with the dual pressures of managing long-term health conditions and navigating an often unforgiving economic landscape, it’s conceivable that feelings of hopelessness and despair might surge.
While these “deaths of despair” highlight the physical toll, they also unfurl a tapestry of deeper societal fissures. Economic instability, lack of access to mental health resources, and the overbearing weight of chronic illness are just some of the contributing factors. It’s evident that these deaths are not just mere numbers but symptomatic of deeper systemic issues, calling for a comprehensive re-evaluation of America’s societal and healthcare priorities.
The Racial and Socioeconomic Gradient in Health Outcomes:
In the vast landscape of American healthcare, disparities continue to emerge when viewed through the lenses of race and socioeconomic status. The Commonwealth Fund, through its detailed studies, provides revealing numbers that underscore this concern.
A concerning finding from the Commonwealth Fund reveals that Black and Hispanic adults are often at the receiving end of these disparities. For instance, the data reveals that 45% of Black and 36% of Hispanic adults were more likely to have cost-related medical non-adherence compared to 28% of their white counterparts. This non-adherence entails either skipping necessary prescriptions, avoiding doctor’s visits, or both, due to the high expenses involved.
Delving into the socioeconomic disparities, it’s not just about racial differences. Economic standing has its influence on healthcare outcomes. According to the Commonwealth Fund, adults with incomes below 200% of the federal poverty level are twice as likely to avoid medical care due to costs when compared to those with incomes at 400% of the federal poverty level or higher.
What’s more, these socioeconomic challenges have an overlay of racial bias. The same Commonwealth Fund data shows that among low-income adults, racial minorities bear a higher burden. For instance, 40% of low-income Black adults and 35% of low-income Hispanic adults reported cost-related medical non-adherence. This, compared to 30% of low-income white adults, clearly showcases the intersectionality of race and economics in healthcare access.
Piecing these figures together, the portrait that emerges is one of pronounced disparity. Black and Hispanic communities, especially those in lower socioeconomic strata, face daunting challenges in accessing affordable, quality healthcare. The overarching implication is evident: a clarion call for systemic reforms that make equitable healthcare a reality, not just a promise.
The Implications of Socioeconomic and Racial Disparities
- Health Inequity leads to Economic Disparity: Health challenges exacerbate economic challenges. Absence from work due to health reasons, coupled with costly medical bills, often drives families into economic hardships, forming a vicious circle. This impact is profound among lower-income families and racial minorities.
- Generational Impact: Healthcare disparities, especially when influenced by race and socioeconomics, can leave generational impacts. Children in communities or families experiencing health challenges are more likely to face health issues themselves, setting the stage for repeated patterns.
- National Productivity and Growth: On a macro level, health disparities can stifle national productivity. A significant portion of the populace grappling with health issues means lesser productive work hours, which can impact the country’s economic trajectory.
- Social Cohesion: Persistent health disparities can sow seeds of mistrust and resentment. When certain groups feel systematically underserved or neglected, it can erode the social fabric, leading to unrest and further sociopolitical challenges.
The Opioid Crisis – A Symptom of Larger Issues:
The opioid crisis, with its devastating effects, is not just a tale of addiction but an intricate web of healthcare shortcomings and societal challenges. The U.S. Congress Joint Economic Committee offers a deep dive into the trajectory of this crisis.
A noteworthy revelation by the U.S. Congress Joint Economic Committee traces the epidemic back to the late 1990s when pharmaceutical companies reassured the medical community that opioid pain relievers were not addictive. The consequent surge in prescriptions led to widespread misuse even before it became apparent that these medications were indeed highly addictive.
The repercussions were immediate and alarming. By 2017, an estimate from the CDC, as cited by the U.S. Congress Joint Economic Committee, showed that 47,600 Americans died as a result of overdosing on opioids. This includes both prescription and illicit opioids.
However, the current scenario paints an even graver picture. As the U.S. Congress Joint Economic Committee highlights, the epidemic is no longer just about prescription opioids. There’s a noticeable surge in deaths due to illegal opioids, specifically heroin and fentanyl. Between 2010 and 2017, heroin-related overdose deaths increased fivefold, while deaths from synthetic opioids, including fentanyl, saw a staggering tenfold increase.
But it’s not just about numbers. The crisis underlines broader healthcare challenges, from overprescription to lack of awareness about addiction risks. Furthermore, it also throws light on deeper societal issues. The prevalence of these drugs in economically depressed areas suggests that many are using them as an escape from the harsh realities of life, a phenomenon that speaks volumes about the country’s socioeconomic challenges.
Bibliography
- Centers for Disease Control and Prevention. 2022, August 31. “Life Expectancy in the U.S. Dropped for the Second Year in a Row in 2021.” https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/20220831.htm.
- Howard, Jacob. 2023, January 31. “US spends most on health care but has worst health outcomes among high-income countries, new report finds.” CNN. https://www.cnn.com/2023/01/31/health/us-health-care-spending-global-perspective/index.html.
- Mole, Beth. 2023, January 31. “US still has the worst, most expensive health care of any high-income country.” Ars Technica. https://arstechnica.com/science/2023/01/us-still-has-the-worst-most-expensive-health-care-of-any-high-income-country/.
- Shmerling, Robert H. 2022, October 20. “Why life expectancy in the US is falling.” Harvard Health Publishing. https://www.health.harvard.edu/blog/why-life-expectancy-in-the-us-is-falling-202210202835.
- The Commonwealth Fund. 2023, January 31. “U.S. Health Care from a Global Perspective, 2022: Accelerating Spending, Worsening Outcomes.” https://www.commonwealthfund.org/publications/issue-briefs/2023/jan/us-health-care-global-perspective-2022.
- United States Congress Joint Economic Committee. 2019, September 5. “Long-Term Trends in Deaths of Despair.” https://www.jec.senate.gov/public/index.cfm/republicans/2019/9/long-term-trends-in-deaths-of-despair.

